Written by: Andra Farcas, MD (NUEM PGY-2) Edited by: Paul Trinquero, MD (NUEM PGY-4) Expert commentary by: Andrew Pirotte, MD
Developing a Post-Intubation Checklist
Multiple studies have shown checklists in medicine can be beneficial. They have been used to reduce rates of catheter-related blood stream infections and ventilator associated pneumonias and to improve team performance in various settings.
In the ED setting, a peri-intubation checklist for trauma patients resulted in more use of rapid sequence intubation and a trend towards improvement in post-intubation sedation rates.[1] This checklist included meds for pre-intubation (pre-treatment, induction, paralytics) and information about which intubation device was used but had only one line for post-intubation medications and did not include other post-intubation safety measures.
One of the few studies that we could find specifically focused on a post-intubation checklist was a MICU study by McConnell, et al. They looked at the proportion of patients who had an ABG drawn within 60 minutes of mechanical ventilation initiation, as well as rates of respiratory acidosis and acidemia. They found that after initiating a post-intubation checklist and timeout, the rates of ABGs increased, which led to earlier recognition of inappropriate ventilation settings.
There are a lot of pre-intubation checklists available for public use. For example, a great podcast/blogpost by Scott Weingart on the topic was developed into a checklist by Jeffrey Siegler and Christ Huntley. Their versions can be found at https://emcrit.org/emcrit/post-intubation-package/.
Our goal was to design a checklist specifically for the post-intubation setting that could potentially be implemented in our emergency department. We took ideas from aforementioned studies and existing checklists, as well as personal experience. In addition to covering a broad array of post-intubation tasks, we wanted to focus especially on post-intubation sedation and initial vent settings. In regards to these important tasks, what we do in the ED matters. Not only are the first few hours a critical period in the course of illness, but there is significant downstream momentum associated with choices made in the Emergency Department.
The SPICE trial showed a link between deep early sedation and prolonged ventilation and increased mortality.[6] Conversely, an analgesia only, no-sedation approach has been shown to reduce time on the ventilator.[7] Consequently, we advocate for an analgesia-first approach. Fentanyl is a commonly used opioid for this purpose because of its rapid onset and short half-life. An easy starting point is a 0.5 - 1mcg/kg fentanyl push, followed by a drip starting at 25mcg/hr and uptitrated by 25mcg every 15-30 minutes (concurrent with another bolus as needed to control pain).
If pain is under control and additional sedation is needed, there are many options. Propofol is commonly used and is easily titratable. Start with a bolus of 5 mcg/kg/min (for 5 min) and start the drip at 5 to 10 mcg/kg/min, increasing by 5-10mcg/kg/min intervals every 5 min as needed (usual range 5-50mcg/kg/min). In the case of hypotension precluding the use of propofol, consider ketamine. Try to avoid benzodiazepines as these have been shown to increase risk of delirium.
Similarly, the initial vent settings that we chose in the ED matter and they can affect duration of ventilation, ICU length of stay, hospital length of stay, and other patient-oriented outcomes.[2] Not all illnesses requiring intubation and mechanical ventilation are the same and consequently vent-settings are not a one size fits all selection. Try to tailor settings to the individual patient and illness and choose one of the following broad strategies[9]:
Lung Protective Strategy (ARDS, lung injury, default for most patients): goal is to minimize additional injury via volutrauma or barotrauma. Set the tidal volume at 6-8cc per kg (of ideal body weight). Soon after intubation, drop Fio2 to 30% and PEEP to 5cm then titrate according to ARDSNet strategy for goal oxygen saturation 88-95%.
Obstructive Strategy (asthma or COPD): goal is to minimize air trapping by maximizing expiration time. Hence, set a low rate (perhaps 10) which will minimize I:E ratio (perhaps 1:4). Tidal volume can be standard 8cc/kg. This strategy may require permissive hypercapnea.
Severe acidosis (DKA, severe sepsis, etc.): Goal is to mimic the pre-intubation minute ventilation. Set the respiratory rate to match pre-intubation rate (usually at least 25-30).
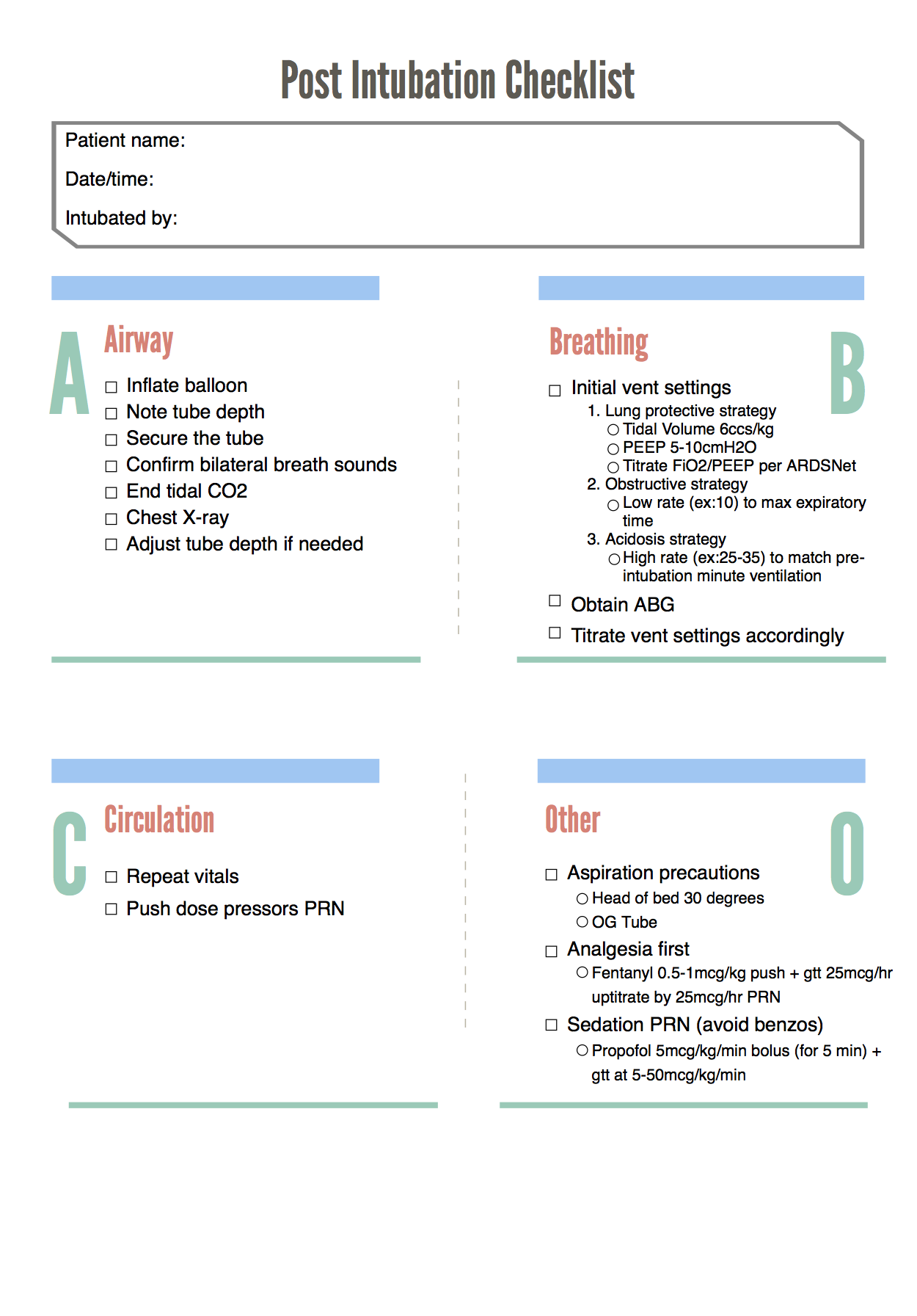
Below is our designed post-intubation checklist:
Expert Commentary
This column highlights the need for optimized post-intubation management. This process requires attention to detail and patient needs. Effective management not only involves delivery of adequate analgesia and sedation, but also efficient titration of the ventilator. Each of these aspects of post-intubation management can be multi-faceted and challenging. To assist with these processes and to simplify tasks, a checklist can be of great value.
Checklists can help create a stepwise clinical approach and trigger timely delivery of individual tasks. Checklists can also help prevent omission of vital steps. A task as simple as a chest X-ray to confirm endotracheal tube placement and positioning can be overlooked in an emergent situation. The checklist provided in the review provides a simple, direct pathway to assist with post-intubation management, and avoid task omission. In addition, this checklist can help emphasize strategies in the post-intubation period. For example, the use of an “analgesic first” pathway for patient comfort following intubation.
As stated in the blog post, evidence now suggests “analgesic first” pathways improve patient outcomes. The clinician should strive to enhance analgesia prior to escalating sedation. Sedation has its role in post-intubation management, but should be employed only if escalated analgesic efforts fail. “Analgesic first” pathways decrease ICU length of stay, decrease complications, and improve outcomes. In addition to managing patient comfort, the clinician must also focus on optimizing ventilation and oxygenation.
Successful ventilator management requires attention to detail and the clinical scenario. Every patient has different ventilation and oxygenation needs. In addition to frequently reevaluating the patient clinically, a common and effective strategy for optimizing a ventilated patient is use of frequent blood gas measurement. Titration of ventilation and oxygenation can be aided greatly with serial blood gas monitoring. The use of blood gas data can also guide the provider utilizing a specific ventilation strategy (eg Lung-protective strategy). Common problems in early post-intubation management include excessive oxygen delivery and hypoventilation. Both of these can be identified by blood gas sampling. Once optimal ventilation and oxygenation is achieved, the clinician can proceed with further diagnostic and stabilization pathways.
Within the airway community, much focus is placed on optimized laryngoscopy and endotracheal tube delivery, no desaturation during intubation, interesting new equipment, etc. However, managing an airway does not conclude with delivery of the endotracheal tube. All clinicians managing airways would benefit greatly from accompanying this enthusiasm for intubation with focused and detailed care (often supplemented by checklists) in the post-intubation period.
Special thanks to Dr. Jordan Kaylor and Dr. Matthew Pirotte
Andrew Pirotte, MD
Department of Emergency Medicine, University of Kansas Hospital
Clinical Assistant Professor, University of Kansas Medical Center
How To Cite This Post
[Peer-Reviewed, Web Publication] Farcas A, Trinquero P (2019, February 11). Post-Intubation Checklist [NUEM Blog. Expert Commentary by Pirotte A]. Retrieved from http://www.nuemblog.com/blog/post-intubation
Other Posts You Might Enjoy
References
Conroy, M.J., Weingart, G.S., Carlson, J.N. Impact of checklists on peri-intubation care in ED trauma patients. American Journal of Emergency Medicine, 2014; 32:541-544.
Fuller, B.M., Ferguson, I.T., Mohr, N.M., Drewery, A.M., Palmer, C., Wessman, B.T. et al. Lung-Protective Ventilation Initiated in the Emergency Department (LOV-ED): A Quasi-Experimental, Before-After Trial. Annals of Emergency Medicine, 2017; 70(3):406-418.
Guthrie, K., Rippey, J. Emergency Department Post-Intubation Checklist. Agency for Clinical Innovation, 2013. https://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0003/273792/emergency-department-post-intubation-checklist-charles-gairdner.pdf. Accessed May 26, 2018.
McConnell, R.A., Kerlin, M.P., Schweickert, W.D., Ahmad, F., Patel, M.S., Fuchs, B.D. Using a Post-Intubation Checklist and Time Out to Expedite Mechanical Ventilation Monitoring: Observational study of a Quality Improvement Intervention. Respiratory Care, 2016; 61(7):902-912.
Nickson, C. Post-intubation care. Life In The Fast Lane, Jan 5 2013. https://lifeinthefastlane.com/ccc/post-intubation-care/. Accessed May 26, 2018.
Shehabi, Y., Bellomo, R., Reade, M., Bailey, M., Bass, F., Howe, B. et al. Early Intensive Care Sedation Predicts Long-Term Mortality in Ventilated Critically Ill Patients. American Journal of Respiratory and Critical Care Medicine, 2012; 186(8):724-731.
Strøm, T., Martinussen, T., Toft, P. A protocol of no sedation for critically ill patients receiving mechanical ventilation: a randomised trial. The Lancet, 2010; 375:475-480
Weingart, S. Podcast 84 – The Post-Intubation Package. EMCrit RACC, Oct 16 2012. https://emcrit.org/emcrit/post-intubation-package/. Accessed May 26, 2018.
Weingart, S. Managing Initial Mechanical Ventilation in the Emergency Department. Annals Of Emergency Medicine, 2016; 68(5):614-61