Author: Kimberly Iwaki, MD (EM Resident Physician, PGY-3, NUEM) // Edited by: Ryan Huebinger, MD (EM Resident Physician, PGY-4, NUEM) // Expert Review: Joseph Posluszny, MD
Citation: [Peer-Reviewed, Web Publication] Iwaki K , Huebinger R (2016, November 8). Understanding Inhalation Injury [NUEM Blog. Expert Review By Posluszny J]. Retrieved from http://www.nuemblog.com/blog/inhalation-injury
Introduction
Smoke inhalation injuries are one of the leading causes of morbidity and mortality in the United States. There are over 23,000 smoke inhalation injuries per year resulting in 5,000-10,000 deaths annually [1]. Smoke inhalation can result in 3 types of injuries: thermal injury, chemical irritation, and systemic toxicity, including carbon monoxide and cyanide toxicity.
Managing the Airway in the Acute Setting
Fig, 1: Suspect inhalation injury when a patient has significant facial burns, singed nasal hairs, and/or carbonaceous sputum. Schmitz BU, Griswold JA. Benumof and Hagberg’s Airway Management: Airway Management in Burn Patients. Saunders, 2013. Online.
When assessing a burned or smoke exposed patient for inhalation injury, start by dividing the respiratory system into two regions: supraglottic and subglottic. In the emergency room or acutely following the burn injury or inhalation, the supraglottic airway should be assessed for current and sustained patency. The supraglottic airway will become edematous from uninhibited heat exchange at the level of the naso- and oropharynx, with the heat denaturing proteins and leading to histamine production. The smoke itself causes nitrous oxide production leading to vasodilation and edema in the upper airway [1]. Classic physical exam findings concerning for supraglottic airway compromise that should prompt consideration of urgent intubation include:
- Singed nasal hairs
- Carbonaceous sputum (Fig. 1)
- Edema/erythema/blisters to oropharynx
- Stridor/wheezing/coughing
- Significant facial or neck burns.
In addition, the physical location in which a patient was burned is important. Patients burned in enclosed spaces (homes and factories vs outdoors) are especially prone to both supraglottic and subglottic airway compromise. In fact, patients with minimal body surface burn but exposures to smoke and particulate matter in an enclosed space can deceptively have an inhalation injury. It is important to note that clinical symptoms of impending airway compromise may be delayed more than 24-36 hours after the initial injury [2]. By the time symptoms of respiratory distress arise, the surrounding edema is substantial and often progresses rapidly. For this reason, intubating early if there is a strong suspicion for significant smoke inhalation is recommended.
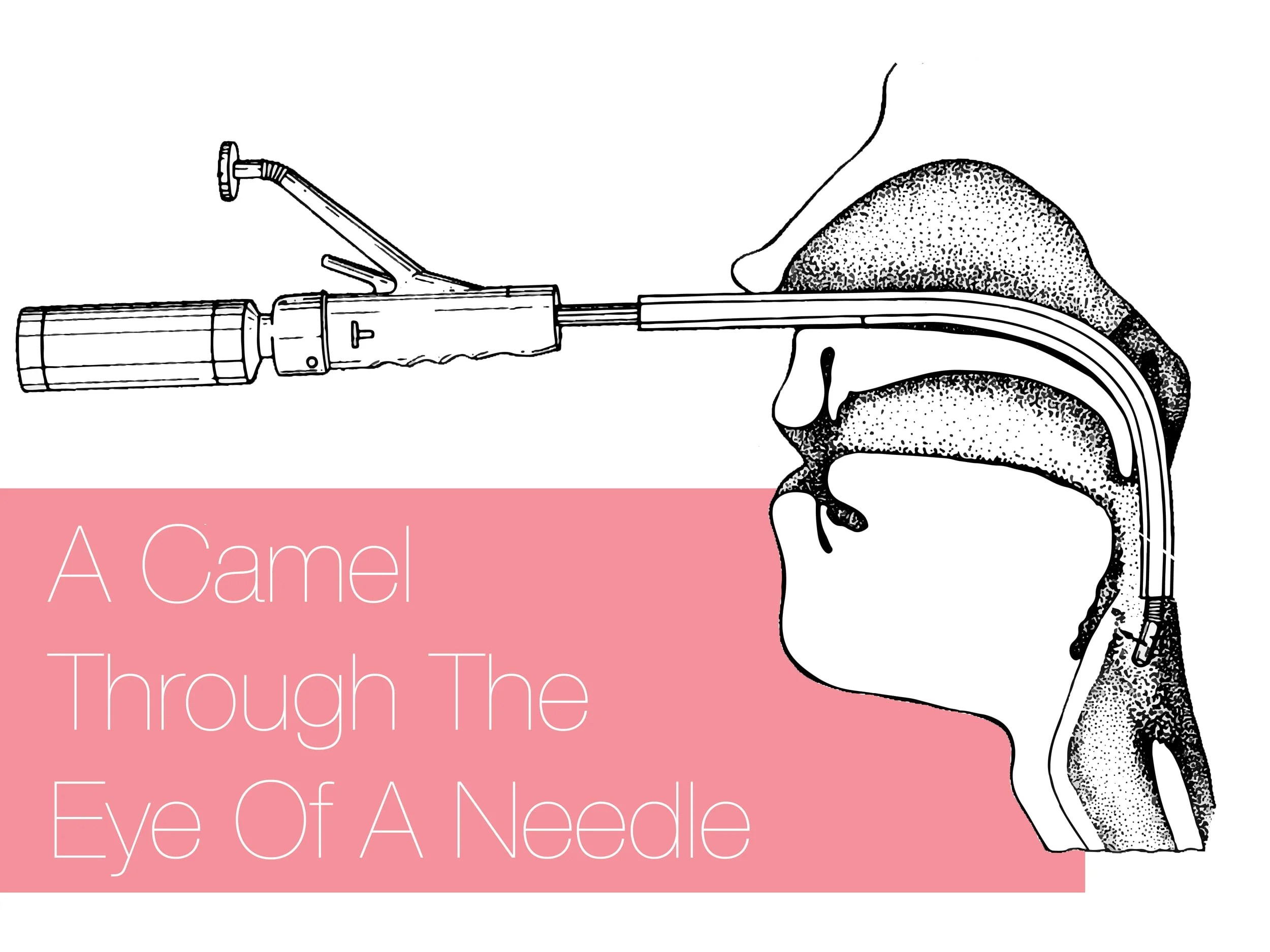
The subglottic portion of the respiratory system is most affected by the smoke itself and the chemicals and particulate matter will irritate, block and inflame the bronchial tree. Given the progressive nature of the inflammatory process, hypoxia and hypoventilation often do not ensue until > 24 hours following the inciting event. At that point, most patients have been transferred to a burn center with specialized protocols for managing inhalation injury. There is no evidence based, single method of managing subglottic inhalation injuries. Therapeutic maneuvers often include frequent pulmonary toilet with bronchoscopy, heightened suspicion for pneumonia and medical therapies. Therapeutic bronchoscopies to remove secretions, debris, and sloughed mucosa may decrease morbidity and shorten durations of mechanical ventilation [8]. Medical therapies are often dispensed as a HAM (heparin, albuterol, Mucomyst) protocol. Bronchodilators including albuterol and racemic epinephrine are imperative [6]. Aerosolized NAC (Mucomyst) works by breaking disulfide bonds of mucoproteins in mucus via its thiol group. Aerosolized heparin is controversial but may decrease morbidity and mortality by limiting fibrin cast formation [7].
From "Fire-Related inhalation Injury [9]"
The following algorithm (right) for early management of inhalation injury provides a great framework for which to assess patients. Patients must be closely monitored and early intubation should be considered if the patient demonstrates hypoxia/hypercapnia or carbon monoxide/cyanide toxicity [3]. Approximately 80% of patients who suffer an inhalation injury will require eventual intubation with aggressive pulmonary hygiene and possible therapeutic bronchoscopy for airway clearance. Therefore, if the decision is made to intubate, an endotracheal tube of 7.5 mm or larger should be used [4].
Complications to anticipate
All inhalation injured patients should be transferred to a burn center once they are stable. In the first 36 hours, the airway should be monitored closely. The patient should be evaluated for carbon monoxide and cyanide poisoning as clinically indicated. Upper and lower airway inflammation with the activation of reactive oxygen species will result in fluid shifts into the alveoli. This will result in worsening edema, deposition of fibrin, and mucosal sloughing which will lead to V:Q mismatch.
Many patients with inhalation injuries have extensive concomitant cutaneous burns, which will require aggressive fluid resuscitation. While the Parkland formula dictates 4mL/kg/% non-superficial burns in the first 24 hours, careful titration of these fluids should be made for patients with co-morbidities (ie CHF) that may lead to pulmonary edema and thus further airway compromise.
The one caveat to early intubation is the frail, geriatric patient with COPD or chronic respiratory issues with a minor burn or inhalation injury. Often, these patients exhibit signs of impending respiratory failure. However, these can be chronic signs and behaviors and intubating these patients can mandate a lifetime of mechanical ventilation and need for tracheostomy. Prior to intubating, consider this clinical scenario and address both the patient’s chronic respiratory disease and goals of care.
Take home points:
- Intubate early. Inhalation injuries can result in delayed aggressive airway edema causing patients to lose their airways quickly, making them difficult to intubate.
- Though aggressive fluid resuscitation is critical in burn victims, titrate the fluids appropriately in patients with co-morbidities that put them at risk for pulmonary edema.
- Inhalation injuries can lead to mucosal sloughing, hypermetabolic states, pneumonia, and ARDS. Pulmonary care includes, but is not limited to, bronchodilators, mucolytic agents, therapeutic bronchoscopies, and chest physiotherapy.
Other Posts You May Enjoy
References
- Rehberg S. Maybauer MO, Enkhbaatar P, Maybauer DM, Yamamoto Y, Traber DL. Pathophysiology, management and treatment of smoke inhalation injury. Expert Rev Respir Med. 2009 Jun 1;3(3):283-297.
- Demling RH. Smoke Inhalation Lung Injury: An Update. Eplasty. 2008; 8: e27.
- Miller K, Chang A. Acute inhalation injury Emerg Med Clin North Am. 2003;21(2):533.
- Rue LW 3rd, Cioffi WG, Mason AD Jr, McManus WF, Pruitt BA Jr. The risk of pneumonia in thermally injured patients requiring ventilator support. J Burn Care Rehabil. 1995 May-Jun;16(3 Pt 1): 262-8.
- Ayres SM, Grenvik A, Holbrook PR, Shoemaker WC. Textbook of Critical Care, 3rd ed. Saunders, 1995. Print.
- Micak RP, Hemdon DN. Total Burn Care: Respiratory Care, 4ed. Saunders, 2009. Print.
- Miller AC, ELamin EM, Suffredini AF. Inhaled anticoagulation regimens for the treatment of smoke inhalation-associated acute lung injury: a systemic review. Crit Care Med. 2014;42(2):413.
- Carr JA, Crowley N. Prophylactic sequential bronchoscopy after inhalation injury: results from a three-year prospective randomized trial. Eur J trauma Emerg Surg. 2013 Apr;39(2):177-83. Epub 2013 Jan 22.
- Sheridan RL. Fire-Related Inhalation Injury. N Engl J Med 2016; 375:464-469.