Author: James Kenny, MD (EM Resident Physician, PGY-2, NUEM) // Edited by: Kory Gebhardt, MD (EM Resident Physician, PGY-4, NUEM)
Citation: [Peer-Reviewed, Web Publication] Kenny J, Gebhardt K (2016, January 26). Purple Urine Bag Syndrome. [NUEM Blog. Expert Peer Review by Schnapp B]. Retrieved from http://www.nuemblog.com/blog/purple-urine-bag-syndrome/
The Case
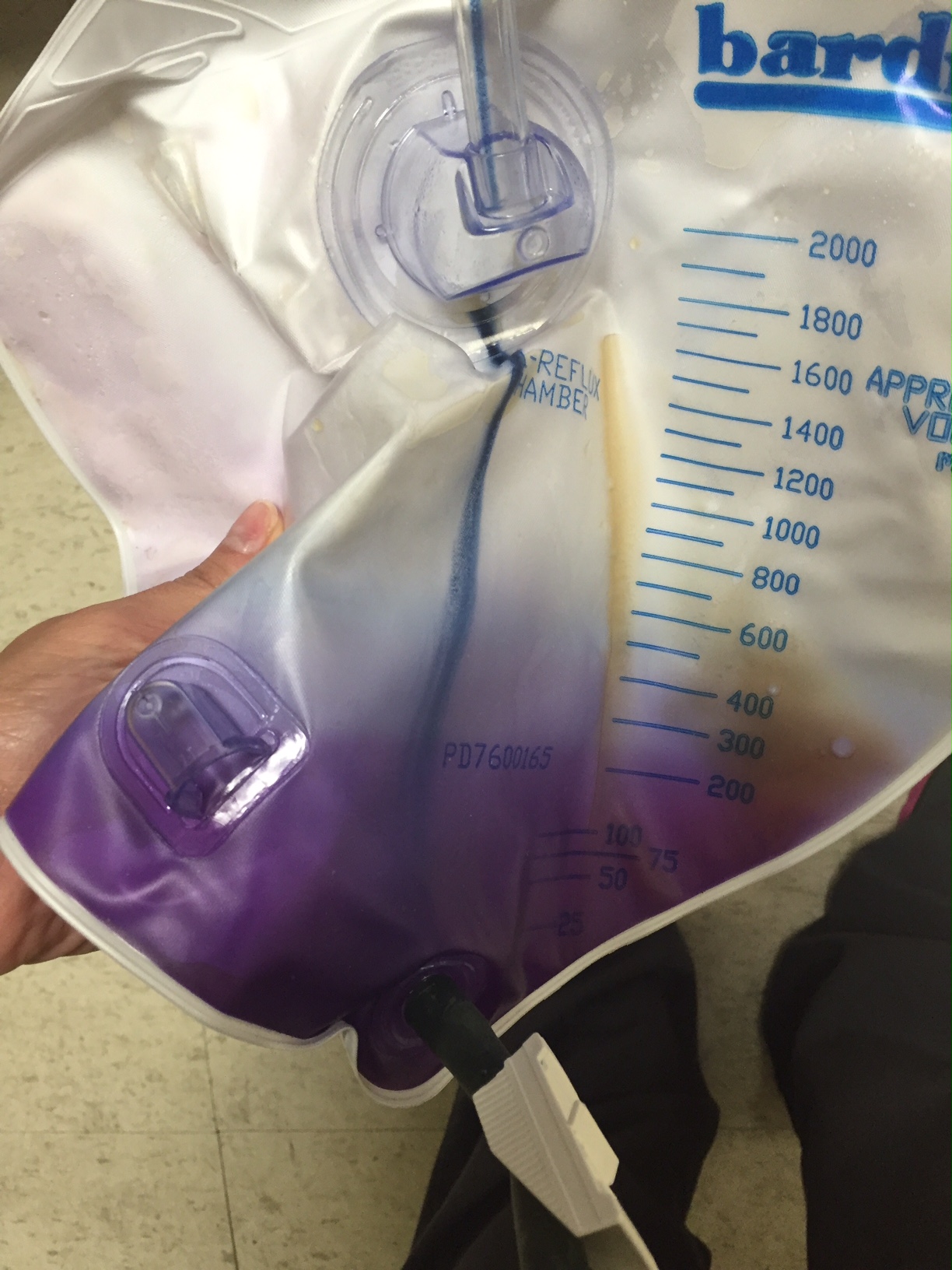
An 75 year-old man with a history of constipation, BPH, and chronic indwelling foley, presented from a skilled nursing facility (SNF) with a chief complaint of purple urine. For the past day it was noted that the color of urine in his foley bag began to take on a purple hue. Concurrently the patient also noted 2 days of lower abdominal discomfort, nausea and intermittent subjective fever.
Vital signs showed a temperature of 101.4F, HR 107, BP 112/65, RR 18 and O2 saturation of 98% on room air. His exam was significant for a fatigued-appearing elderly man with minimal suprapubic tenderness, otherwise unremarkable. An image of his foley bag is displayed (left).
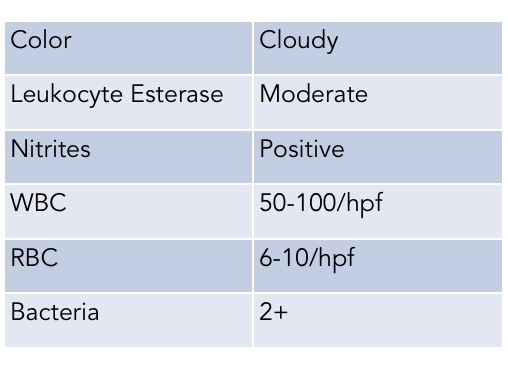
A urinalysis (below) was obtained concerning for urinary tract infection and given the systemic symptoms a diagnosis of pyelonephritis was made. The patient was admitted and started on IV ceftriaxone. A urine culture was sent.
Pathophysiology
Purple Urine Bag Syndrome (PUBS) is a rare condition that is associated with an otherwise common disease process: bacterial urinary tract infection.
Typically, PUBS is associated with gram-negative UTIs, but requires certain circumstances to occur. It is most frequently seen in elderly, ill females (though it also occurs in males) who tend to be chronically catheterized and constipated. Patients with ileal diversions have also been reported to develop this syndrome.
It is thought that constipation predisposes patients to this condition as it promotes bacterial overgrowth and this high bacterial load plays an important part of the pathophysiology. This change in gastrointestinal flora allow dietary tryptophan to be metabolized to indole, which is subsequently metabolized to indoxyl sulphate in the liver. This compound is then excreted in the urine where the bacteria causing the infection catalyze the conversion of indoxyl sulphate into indoxyl. In alkaline environments, the indoxyl is then further converted to the pigmented compounds indigo blue and indirubin, which combine to contribute to the purple discoloration (See sequence below).
Metabolic Pathways of Purple Urine Bag Syndrome: Adopted from chart originally published in Purple Urine Bag Syndrome: A Rare and Interesting Phenomenon. South Med J. 2007;100(10):1048-1050.
Microbiology
Bacteria commonly grown in the urine culture of patients with PUBS include Escherichia coli, Proteus mirabilis, Klebsiella pneumoniae, Enterococcus species, Pseudomonas aeruginosa, Citrobacter species, and several others.
Treatment
While visually alarming, the purple discoloration is fairly benign and management revolves around treatment of the underlying condition. Most often, successful treatment of the UTI and exchange of the catheter typically resolves the condition.
Case Resolution
The urine culture grew 100,000 colonies of Proteus mirabilis susceptible to ceftriaxone. The patient was eventually discharged home on hospital day #3 with cephalexin for 14 days.
Take Home Points
- PUBS is a rare presentation of urinary tract infection predominately in elderly with a history of constipation and chronic catheterization
- The pathophysiology of PUBS is not completely understood but is related to bacterial overgrowth in the gut and conversion of tryptophan to urinary pigments through a complex series of reactions
- The management of PUBS is focused on treatment of the underlying urinary tract condition which includes antibiotic therapy covering the appropriate microflora and foley catheter exchange if applicable
Expert Review
Thanks for this great and informative post on Purple Urine Bag Syndrome. As you mention, although its etiology is not completely understood, it is thought that the constipation allows additional time for gut bacteria to digest tryptophan from the diet into indole, which is further converted into red and blue pigment by the enzymes found in some bacteria in the urine of the chronically catheterized. This explanation does not completely explain the phenomenon however, as some patients have been found with purple urine that lacks these pigments.
While Purple Urine Bag Syndrome is rare (the exact incidence in unknown), urine in colors beyond the usual yellow is much less so.
- Blue urine, which may be mistaken for purple, is associated with the use of methylene blue, sildenafil, B vitamins or even rare conditions like porphyria or Drummond’s syndrome.
- Green urine is classically associated with pseudomonas infection although more commonly seen today with propofol administration (although propofol can also cause white or pink urine!). Medications with phenol groups can also cause green urine, including promethazine and cimetidine, as well as non-phenol medications like metoclopramide and indomethacin.
- Orange urine can be seen with the use of medications like phenazopyridine, rifampin, warfarin and sulfasalazine.
Additionally, brightly colored food products, with or without dye, are a common cause of urine of nearly any color. A detailed history with a focus on recent ingestions and medications is often helpful in elucidating the cause of the color change.
Regardless of the color of the discolored urine, from an emergency medicine perspective, the important thing to remember is to identify and address the underlying cause (in the case of PUBS, usually a UTI and constipation). While abnormally colored urine may be alarming to the patient and caregivers, it is rarely dangerous in and of itself. If the cause is thought to be related to medications or foods, simple reassurance that urine discoloration can be normal may be of tremendous benefit to the patient.
Benjamin Schnapp, MD
Medical Education Fellow; Instructor; Department of Emergency Medicine, Northwestern University, Feinberg School of Medicine
References
- Yaqub S, Mohkum S, Mukhtari KN. Purple urine bag syndrome: A case report and review of literature. Indian J Nephrol, 2013; 23(2): 140–142.
- Vallejo-Manzur F, Mireles-Cabodevila E, Varon J. Purple urine bag syndrome. AJEM, 2005; 23: 521–524.
- Harun NS et al. Purple Urine Bag Syndrome: A Rare and Interesting Phenomenon. South Med J. 2007; 100(10): 1048-1050.